Arc de Triomphe, sebuah monumen megah yang berdiri di pusat kota Paris, memiliki sejarah yang kaya dan menarik. Transisi dari masa lalu ke masa kini, pembangunan monumen ini dimulai pada tahun 1806 atas perintah Napoleon Bonaparte sebagai tanda penghormatan kepada tentara Prancis yang berjuang dalam perang. Dengan tinggi mencapai 50 meter, kehadira
MET Gala 2024 Extravaganza: Unveiling the Spectacular Showcase of Fashion’s Finest Night
The MET Gala, often dubbed “the Oscars of the East Coast,” is not merely a night of opulence and style; it is a barometer for the fashion industry’s dynamism and a spotlight on its artistic ingenuity. This annual event, hosted by the Metropolitan Museum of Art’s Costume Institute in New York City, brings together the [&helli
Building a Home Gym: Transform Your Space Into an Empowering Fitness Sanctuary
With the increasing appeal of comfort and individualized fitness, the concept of a home gym has been approaching for some time. Even with some essential planning, you may transform your gym fit for any desired workouts. This gym may be a cost-effective substitute for expensive gym memberships and full-scale sessions or be intended to truly [&hellip
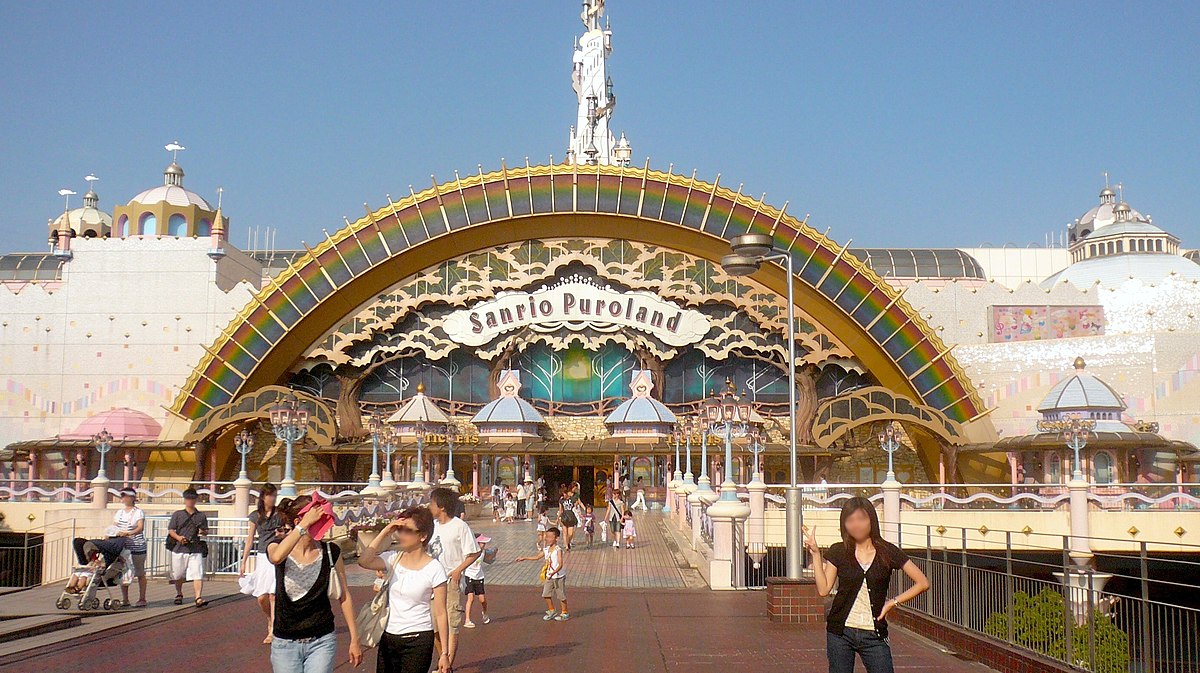
Exploring Sanrio Puroland: A World of Hello Kitty and Friends
Sanrio Puroland, located in Tama New Town, Tokyo, Japan, is a whimsical indoor theme park dedicated to the beloved characters created by Sanrio, including the iconic Hello Kitty. With its vibrant attractions, live shows, and immersive experiences, Sanrio Puroland offers visitors of all ages the chance to step into a fantastical world filled with cu
Potato Wedges Around the World: Discovering Unique Regional Variations
Potato wedges are a beloved snack and side dish enjoyed globally. Cut from whole potatoes with their skin on, these chunky slices are either baked or fried to achieve a crispy exterior and a fluffy interior. Loved for their simple yet satisfying nature, potato wedges serve as a versatile companion to many dishes, ranging from […]